Glycemic Index Decoded: Why Some Carbs Make You Hungrier Than Others
The Science Behind Food Cravings, Metabolic Slowdown, and Why Your Breakfast Choice Could Affect Your Dinner Decisions
Not all carbohydrates are created equal. In fact, kidney beans and jelly beans—both rich in carbs—can have dramatically different effects on your body despite sharing similar-sounding names. To understand why, we need to dive into the fascinating world of the glycemic index and uncover how different carbohydrates influence our hunger, metabolism, and health.
The Birth of a Revolutionary Concept
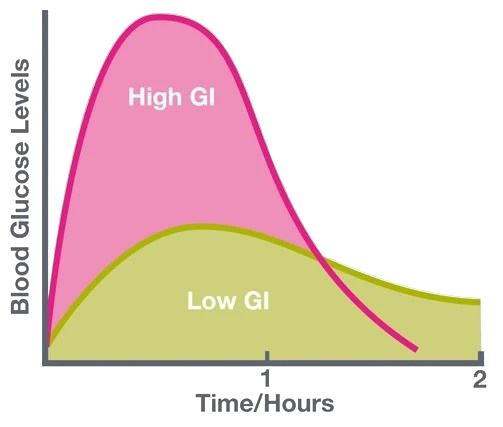
The glycemic index (GI) ranks carbohydrates on a scale of 0-100 based on how quickly they raise blood sugar levels after consumption. Foods with a high GI (>70) are rapidly digested and cause sharp spikes in blood glucose and insulin, while foods with a low GI (<55) are digested more gradually, resulting in smaller, more sustained increases.
The Science of Starch: Why Physical Structure Matters
Think of it like this: high-GI foods are like pouring gasoline on a fire—they create an immediate, intense burst of energy that quickly burns out. Low-GI foods, on the other hand, are more like adding logs to a fireplace—they provide a steady, enduring heat that lasts much longer.
Want to experience this difference firsthand? Try this simple experiment:
Take a bite of bread and chew thoroughly without swallowing. Notice how it gradually tastes sweeter and sweeter? That's because the starch-digesting enzymes in your saliva are breaking down the starch into sugar in real-time.
Now try the same with cooked spaghetti. You might need to chew for two hours to achieve the same sweetness you got from bread in just ten minutes! And if you were to try this with whole wheat berries? You'd be chewing all day.
This experiment illustrates a fundamental principle: the physical structure of food dramatically influences how quickly it's digested. Bread is filled with tiny air bubbles that allow digestive enzymes to easily access more surface area, rapidly converting starch to sugars. Pasta, being more compact, forces enzymes to work their way in from the edges, significantly slowing digestion.
The Three Categories of Starch
When discussing carbohydrates, particularly starches (found in foods like potatoes, rice, bread, and pasta), nutritional scientists now categorize them into three main types:
Rapidly Digestible Starch (RDS): The sprinter of the starch world—digested quickly and causing rapid glucose spikes.
Slowly Digestible Starch (SDS): The marathon runner—broken down gradually, resulting in a more moderate and sustained glucose response.
Resistant Starch (RS): The rebel—passes through the small intestine largely undigested, acting more like dietary fiber than a typical starch.
Research shows that foods containing slowly digestible starch have a lower glycemic index, independent of other nutrients like fat and fiber (Englyst et al., 2003). This understanding has revolutionized how we evaluate carbohydrate quality beyond simple "carbs are bad" thinking.
The Neurological Impact: How High-GI Foods Hijack Your Brain
High-glycemic foods don't just affect your waistline—they actually light up your brain's reward centers. In a revealing study, researchers placed participants in brain scanners after consuming high-GI versus low-GI meals (matched for calories and taste). The results were striking: significantly greater activation occurred in brain regions associated with reward and craving following the high-GI meal (Lennerz et al., 2013).
This finding helps explain why most foods identified as potentially "addictive" in research tend to be high-glycemic options. It's not just the presence of refined carbs like white flour and sugar that makes these foods problematic—it's the speed at which they're absorbed that predicts their addictive potential.
The Appetite Effect: The Breakfast That Makes You Hungrier Later
In a particularly illuminating study, children who ate high-GI breakfast cereals (Corn Flakes, Coco Pops, Rice Krispies) consumed significantly more food at a buffet lunch compared to when they ate the same number of calories from lower-GI oatmeal—even when the oatmeal had added sugar! The lower-GI breakfast resulted in approximately 100 fewer calories consumed at lunch (Warren et al., 2003).
This demonstrates a crucial mechanism: low-GI foods improve satiety and potentially reduce overall calorie intake throughout the day. When we consume high-GI foods, the rapid rise and subsequent crash in blood sugar levels can trigger premature hunger and overeating at subsequent meals.
Metabolic Consequences: Fat Burning and Energy Expenditure
Enhanced Fat Oxidation
When people eat a low-GI meal (like All-Bran cereal with fruit) and exercise three hours later, they burn more fat than after consuming the same number of calories from a high-GI meal (like Corn Flakes and white bread). This enhanced fat oxidation occurs not only during exercise but even during rest (Stevenson et al., 2009).
Preventing Metabolic Slowdown
One reason weight loss is so challenging is that our bodies defend against fat loss by slowing metabolic rates. However, research shows that on a low-GI diet, metabolic rates don't slow down as much. In one groundbreaking study, participants' metabolisms slowed by 96 calories per day after losing about twenty pounds on a low-GI diet, compared to 176 calories on a higher-GI diet—an 80-calorie difference that's equivalent to walking an extra mile daily without any additional effort (Ebbeling et al., 2012).
The reverse is also true: when overfed on a high-GI diet, people store more fat than those eating the same excess calories on a low-GI diet. The difference can amount to about 40% less fat gain—approximately a pound of fat per week—despite identical calorie consumption.
The Resistant Starch Revolution: A Special Category of Carbs
Resistant starch deserves special attention as it acts more like soluble fiber than typical starch. It passes through your digestive tract undigested, feeding beneficial gut bacteria and improving your microbiome. Because it doesn't get digested, it helps reduce the glycemic response after a meal and even creates a "second meal effect," improving glucose responses at subsequent meals (Higgins, 2004).
Resistant starch comes in several forms:
Type 1: Physically inaccessible starch found in whole-kernel grains, seeds, and legumes.
Type 2: Present in unripe bananas and raw potatoes.
Type 3: Forms when starchy foods are cooked and then cooled (like in potato salad or day-old rice).
Type 4: Chemically modified starch.
Type 5: Forms when starch interacts with lipids.
The easiest ways to increase resistant starch in your diet include eating cashews, slightly underripe bananas, and cooling cooked rice or potatoes before consumption.
Putting Theory Into Practice: Low vs. High GI Foods
Now that we understand the science, let's identify which foods fall into which categories:
The High-GI Hall of Shame (GI ≥70)
These foods typically cause rapid blood sugar spikes:
White bread (GI 100)
Cornflakes and other processed breakfast cereals
Pretzels
White potatoes (particularly when mashed or baked)
Sweet potatoes (depending on preparation)
Sugar-sweetened beverages
Bakery items (croissants, scones, muffins)
Most candies (Skittles, Swedish Fish)
Beer
Even some fruits with higher sugar content, like watermelon and pineapple, can have higher GI values, though they offer beneficial nutrients and fiber that partially offset this effect.
The Low-GI All-Stars (GI ≤55)
These foods promote more stable blood sugar levels:
Non-starchy vegetables (spinach, broccoli, tomatoes, cucumbers)
Most fruits, especially berries, apples, and oranges
Legumes (lentils, chickpeas, beans)
Whole intact grains (steel-cut oats, quinoa, barley)
Dairy products (skim, low-fat, full-dat milk, greek yogurt)
Nuts and seeds
Avocado
Mushrooms
Whole grain bread
Fish and shellfish
Chicken, turkey, and other poultry
Eggs
Beef and pork
Low-GI Chinese Options (GI <55)
Vegetable-forward dishes: Stir-fried vegetables with tofu, Chinese broccoli (Gai Lan), and cucumber salad all have minimal impact on blood sugar
Mushroom dishes: Shiitake or wood ear mushrooms are not only delicious but have very low GI values (under 15)
Protein-centered meals: Steamed fish with ginger and scallions, or other protein-focused dishes with limited carbohydrates
Bean sprouts: A common addition to many dishes, these have a low GI (around 25-35)
Soup bases: Hot and sour soup generally has a low GI (around 30-40) due to its protein content and minimal starch
Medium-GI Chinese Options (GI 55-69)
Dumplings: Steamed varieties (depending on filling) typically fall in the medium range (around 55-65)
Tofu dishes: Mapo tofu served with small amounts of rice offers a moderate glycemic impact (around 50-60)
Congee: This rice porridge, especially when prepared with vegetables and protein, has a medium GI (around 50-65)
Brown rice: When available as an alternative to white rice, it offers a more moderate glycemic response (around 50-55)
Glass noodles: Made from mung beans, these have a lower impact than wheat-based noodles (around 45-55)
High-GI Chinese Options (GI ≥70)
White rice: The staple of many Chinese meals has a high GI (around 70-80)
Fried rice: Even higher than plain white rice due to the breakdown of starches during cooking (around 70-90)
Wheat noodles: Egg noodles and wheat-based varieties have high GI values (around 65-80)
Sweet sauces: Dishes with sweet and sour, honey-glazed, or hoisin sauces can spike blood sugar rapidly (GI 70-90+)
Fried appetizers: Spring rolls, egg rolls, and similar items typically have high GI values (70-85)
This doesn't mean you need to avoid your favorite Chinese restaurant. Strategic ordering—focusing on vegetable dishes, choosing brown rice when available, limiting sweet sauces, and emphasizing protein—can significantly lower the glycemic impact of your meal while still allowing you to enjoy the rich flavors of Chinese cuisine.
The Weight Loss Connection: Clinical Evidence
Between the enhanced satiety effects and metabolic benefits of low-GI foods, it's not surprising that randomized controlled trials show greater body fat loss with lower-GI diets. However, what might surprise you is that the evidence for substantial, long-term weight loss with low-GI interventions is somewhat modest.
The Cochrane Collaboration, often considered the gold standard in evidence-based reviews, concluded that "lowering the glycaemic load of the diet appears to be an effective method of promoting weight loss," but the additional benefit typically amounts to just a few extra pounds over weeks or months (Thomas et al., 2007).
Even in the DIOGENES trial, a large European study examining weight maintenance after significant weight loss, those following a lower-GI diet regained about two pounds less weight at six months compared to those on a high-GI diet. However, this advantage largely disappeared by the one-year mark (Larsen et al., 2010).
Why don't we see more dramatic results? One crucial factor is adherence. In controlled feeding studies where scientists can ensure participants follow prescribed diets exactly, the glycemic load can be dropped by 70%. In real-world studies where people simply receive dietary recommendations, the actual difference in glycemic load between "high" and "low" GI groups may be as little as 3%.
As the saying goes: foods only work if you eat them.
The Pharmaceutical Evidence: Acarbose Trials
One of the challenges in nutrition research is isolating the specific effects of a single dietary change. Many high-GI foods are highly processed and fiber-depleted, so when you replace them with low-GI alternatives like beans and fruit, you're changing multiple variables simultaneously.
This is where medication studies provide interesting insight. Acarbose is a drug that partially blocks sugar- and starch-digesting enzymes in the digestive tract, essentially transforming a high-GI meal into a low-GI meal without changing the foods themselves. Weight-loss trials with acarbose offer compelling evidence that simply lowering dietary glycemic load may indeed be beneficial for weight management (DiNicolantonio et al., 2015).
Practical Strategies for Everyday Eating
Based on the science we've explored, here are practical ways to apply this knowledge:
Choose whole, intact grains over refined ones: Opt for steel-cut oats instead of instant oatmeal, brown rice over white rice, and whole grain bread over white bread.
Eat more legumes: Beans, lentils, and chickpeas are nutritional powerhouses with exceptionally low glycemic impacts.
Cook pasta al dente: Slightly undercooked pasta has a lower GI than fully cooked pasta.
Try the "cook and cool" method: Cooling cooked starches like potatoes and rice (even if you reheat them later) increases their resistant starch content.
Add acid to meals: Vinegar, lemon juice, and other acidic ingredients can lower the glycemic response of a meal.
Include protein and healthy fats: These nutrients slow digestion and moderate blood sugar responses when consumed alongside carbohydrates.
Conclusion: Beyond the Glycemic Index
The evidence clearly shows that the quality of carbohydrates matters at least as much as the quantity. Low-GI foods offer advantages for appetite control, fat burning, and metabolic health that extend beyond their calorie content.
While the glycemic index shouldn't be your only consideration when choosing foods (nutrient density, fiber content, and overall diet pattern matter too), it provides a useful framework for making carbohydrate choices that support long-term health and weight management.
As with most aspects of nutrition, the key isn't eliminating entire food groups but making strategic swaps that move your overall dietary pattern in a healthier direction. By understanding the science behind the glycemic index, you're equipped to make informed decisions about the carbohydrates you consume—potentially transforming not just your next meal, but your long-term health trajectory.
References
Ebbeling, C. B., Swain, J. F., Feldman, H. A., Wong, W. W., Hachey, D. L., Garcia-Lago, E., & Ludwig, D. S. (2012). Effects of dietary composition on energy expenditure during weight-loss maintenance. JAMA, 307(24), 2627-2634.
Englyst, K. N., Vinoy, S., Englyst, H. N., & Lang, V. (2003). Glycaemic index of cereal products explained by their content of rapidly and slowly available glucose. British Journal of Nutrition, 89(3), 329-340.
Higgins, J. A. (2004). Resistant starch: metabolic effects and potential health benefits. Journal of AOAC International, 87(3), 761-768.
Jenkins, D. J., Wolever, T. M., Taylor, R. H., Barker, H., Fielden, H., Baldwin, J. M., Bowling, A. C., Newman, H. C., Jenkins, A. L., & Goff, D. V. (1981). Glycemic index of foods: a physiological basis for carbohydrate exchange. The American Journal of Clinical Nutrition, 34(3), 362-366.
Larsen, T. M., Dalskov, S. M., van Baak, M., Jebb, S. A., Papadaki, A., Pfeiffer, A. F., Martinez, J. A., Handjieva-Darlenska, T., Kunešová, M., Pihlsgård, M., Stender, S., Holst, C., Saris, W. H., & Astrup, A. (2010). Diets with high or low protein content and glycemic index for weight-loss maintenance. New England Journal of Medicine, 363(22), 2102-2113.
Lennerz, B. S., Alsop, D. C., Holsen, L. M., Stern, E., Rojas, R., Ebbeling, C. B., Goldstein, J. M., & Ludwig, D. S. (2013). Effects of dietary glycemic index on brain regions related to reward and craving in men. The American Journal of Clinical Nutrition, 98(3), 641-647.
Stevenson, E. J., Williams, C., Mash, L. E., Phillips, B., & Nute, M. L. (2009). Influence of high-carbohydrate mixed meals with different glycemic indexes on substrate utilization during subsequent exercise in women. The American Journal of Clinical Nutrition, 84(2), 354-360.
Thomas, D. E., Elliott, E. J., & Baur, L. (2007). Low glycaemic index or low glycaemic load diets for overweight and obesity. Cochrane Database of Systematic Reviews, (3), CD005105.
Warren, J. M., Henry, C. J., & Simonite, V. (2003). Low glycemic index breakfasts and reduced food intake in preadolescent children. Pediatrics, 112(5), e414-e419.
DiNicolantonio, J. J., Bhutani, J., & O'Keefe, J. H. (2015). Acarbose: safe and effective for lowering postprandial hyperglycaemia and improving cardiovascular outcomes. Open Heart, 2(1), e000327.